“My father developed type 2 diabetes in his late 30’s and died at age 51 of a stroke shortly after I finished medical school,” said Chris K. Guerin MD, FACE, FNLA, a board-certified endocrinologist at Tri-City Medical Center. “I knew then that I would devote my professional career to helping people with diabetes avoid complications and premature death. Most people don’t realize it, but people with diabetes are markedly at risk of strokes, heart attacks and premature kidney failure.”
“My father developed type 2 diabetes in his late 30’s and died at age 51 of a stroke shortly after I finished medical school,” said Chris K. Guerin MD, FACE, FNLA, a board-certified endocrinologist at Tri-City Medical Center. “I knew then that I would devote my professional career to helping people with diabetes avoid complications and premature death. Most people don’t realize it, but people with diabetes are markedly at risk of strokes, heart attacks and premature kidney failure.”
Although type 2 diabetes mellitus (T2DM) tends to run in families, lifestyle and environmental factors can also play a role. “It’s like the analogy, genetics loads the gun, but the environment pulls the trigger,” said Dr. Guerin who has been with Tri-City for almost 40 years. “There is nothing patients can do about their genetics, but they can control their diabetes and other associated risk factors to prevent these devastating health conditions.”
To stay in control, patients should start by learning as much as they can about T2DM, a condition in which cells don’t respond the way they should to the insulin produced in the pancreas. Insulin allows blood glucose, derived from the foods we eat, to enter the cells where it is converted to energy. When it cannot get in, it builds up in the bloodstream causing the pancreas to go into overdrive and eventually, it cannot make enough insulin to keep up. Credible sources, such as the American Diabetes Association, the National Institute of Diabetes and Digestive and Kidney Diseases, Medline Plus and the Centers for Disease Control and Prevention offer a wealth of accurate and up-to-date information about this insulin resistance disease.
“Unfortunately, there is a lot of misinformation about T2DM, such as it can be managed without medication or it’s only about glucose control,” added Dr. Guerin. “By the time diabetes is diagnosed, patients have already lost more than 50% of their beta cell function (the cells in the pancreas that make insulin) and require medications or insulin. Patients must also keep their LDL-cholesterol levels in check.”
Oral medications are crucial to help patients, who can still produce their own insulin, achieve optimal blood glucose levels. Different types of medications, including metformin, sulfonylureas, alpha-glucosidase inhibitors and others may need to be taken in combination over time. Some patients may require insulin injections if their bodies don’t make or use enough of it on their own.
 “Lifestyle changes, such as weight loss, healthy eating and physical activity are the cornerstone of all of our therapies;” said Dr. Guerin. “I am passionate about a whole food, plant-based diet that includes non- or minimally-processed foods, like whole grains, fruits, vegetables and legumes. I encourage patients to avoid highly refined grain products such as white rice or flour, and foods containing added sugars or artificial sweeteners or added fat or oils. Working with a TCMC registered dietician can be helpful in planning diabetic-friendly meals.”
“Lifestyle changes, such as weight loss, healthy eating and physical activity are the cornerstone of all of our therapies;” said Dr. Guerin. “I am passionate about a whole food, plant-based diet that includes non- or minimally-processed foods, like whole grains, fruits, vegetables and legumes. I encourage patients to avoid highly refined grain products such as white rice or flour, and foods containing added sugars or artificial sweeteners or added fat or oils. Working with a TCMC registered dietician can be helpful in planning diabetic-friendly meals.”
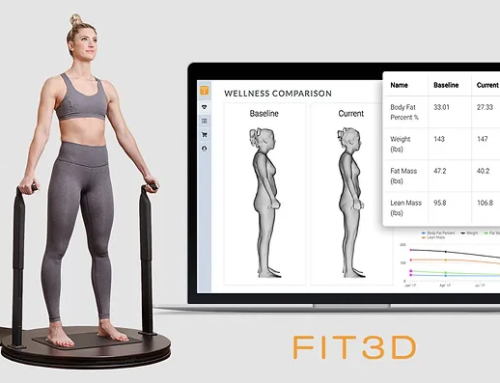
As part of its COASTAL Commitment partnership with the Move Your Feet Before You Eat®! foundation, TCMC encourages North County residents to incorporate regular physical fitness into their daily lives to address prevalent chronic conditions such as cardiovascular disease, diabetes and obesity.
“I feel people are developing T2DM at an alarming rate, especially young people,” added Dr. Guerin. “When I first started practicing, I would only see a handful of women each year with gestational diabetes – now I see one to two women per week.”
A 2022 CDC report indicates that 37.3 million people in the US have diabetes and an estimated 1.4 million new cases of diabetes were diagnosed among people ages 18 and older in 2019. American Indian or Alaska Native, non-Hispanic Black, Hispanic, and non-Hispanic Asian people are more likely to be diagnosed with diabetes than non-Hispanic White people.
“Cultural biases have developed, which is increasing the prevalence of T2DM,” added Dr. Guerin. “For example, in some cultures, denial is so strong that proper treatment is delayed much too long and complications have already developed. The patients’ friends and family members then think that complications are inevitable, and they give up. We need to change this misperception, as early treatment has been shown to markedly decrease the risks of complications.”
This report also found that during the pandemic, diabetes emerged as an underlying condition that increased the chance of severe illness. Nearly four in 10 adults who died from COVID-19 in the US also had diabetes. Other studies have also shown that COVID-19 can increase a person’s risk of developing diabetes, up to 12 months after infection, compared to those who never had the disease.
“These findings are beginning to show a correlation between COVID-19 and diabetes,” said Dr. Guerin. “There is still much research that needs to be done to determine what may be causing an increase in diabetes in COVID-19 long haulers. For now, proper medication management, glucose monitoring, lifestyle changes and vaccinations are critical for anyone living with T2DM, as are maintaining regular visits with your primary care physician or endocrinologist.”
To learn more about the primary care services offered at Tri-City Medical Center, call 855-222-8262 to be referred to a Tri-City Primary Care physician.
To learn more about the diabetes services offered at Tri-City Medical Center, call 855-222-8262 to be referred to an endocrinologist.